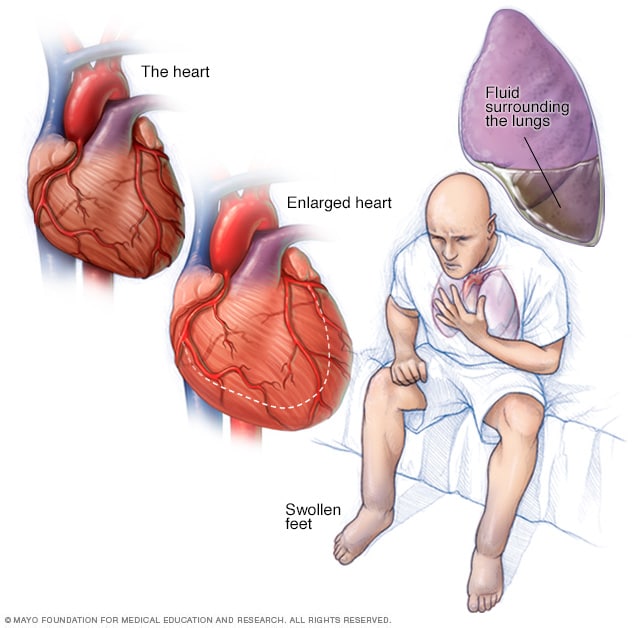
Heart failure occurs when your heart muscle doesn't pump blood as well as it should. When your heart doesn't pump enough blood to meet your needs, blood often backs up and causes fluid to build up in your lungs (congest) and in your legs, causing your legs to swell and turn blue from lack of oxygenated blood flow (cyanosis). This fluid in your lungs can make you short of breath. Some types of heart failure can lead to an enlarged heart.
Definition
Heart failure, sometimes known as congestive heart failure, occurs when your heart muscle doesn't pump blood as well as it should. Certain conditions, such as narrowed arteries in your heart (coronary artery disease) or high blood pressure, gradually leave your heart too weak or stiff to fill and pump efficiently.
Not all conditions that lead to heart failure can be reversed, but treatments can improve the signs and symptoms of heart failure and help you live longer. Lifestyle changes — such as exercising, reducing salt in your diet, managing stress and losing weight — can improve your quality of life.
One way to prevent heart failure is to control conditions that cause heart failure, such as coronary artery disease, high blood pressure, diabetes or obesity.
Symptoms
Heart failure can be ongoing (chronic), or your condition may start suddenly (acute).
Heart failure signs and symptoms may include:
- Shortness of breath (dyspnea) when you exert yourself or when you lie down
- Fatigue and weakness
- Swelling (edema) in your legs, ankles and feet
- Rapid or irregular heartbeat
- Reduced ability to exercise
- Persistent cough or wheezing with white or pink blood-tinged phlegm
- Increased need to urinate at night
- Swelling of your abdomen (ascites)
- Sudden weight gain from fluid retention
- Lack of appetite and nausea
- Difficulty concentrating or decreased alertness
- Sudden, severe shortness of breath and coughing up pink, foamy mucus
- Chest pain if your heart failure is caused by a heart attack
When to see a doctor
See your doctor if you think you might be experiencing signs or symptoms of heart failure. Seek emergency treatment if you experience any of the following:
- Chest pain
- Fainting or severe weakness
- Rapid or irregular heartbeat associated with shortness of breath, chest pain or fainting
- Sudden, severe shortness of breath and coughing up pink, foamy mucus
Although these signs and symptoms may be due to heart failure, there are many other possible causes, including other life-threatening heart and lung conditions.
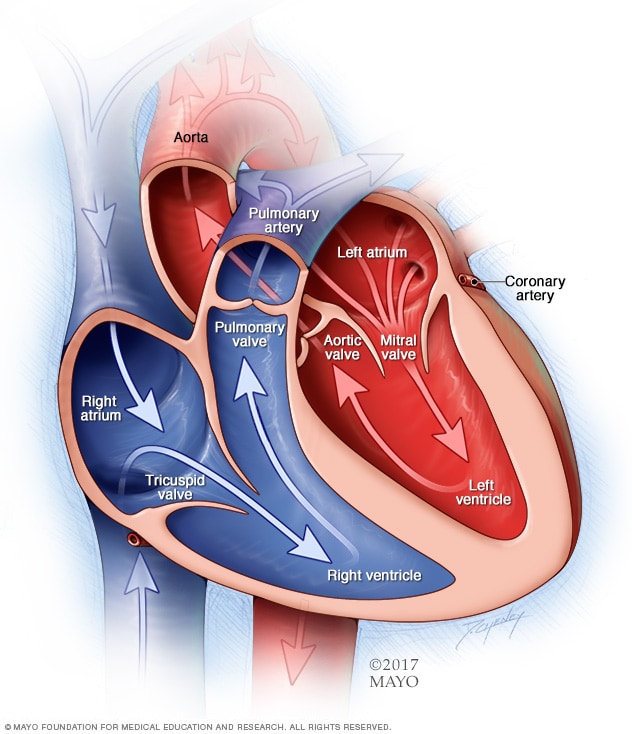
A normal heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of your heart. The heart valves, which keep blood flowing in the right direction, are gates at the chamber openings.
Causes
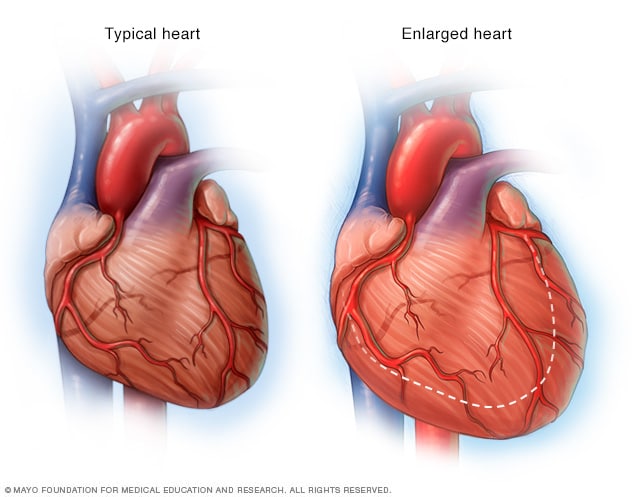
As your heart weakens, such as in heart failure, it begins to enlarge, forcing your heart to work harder to pump blood to the rest of your body.
Heart failure often develops after other conditions have damaged or weakened your heart. However, the heart doesn't need to be weakened to cause heart failure. It can also occur if the heart becomes too stiff.
In heart failure, the main pumping chambers of your heart (the ventricles) may become stiff and not fill properly between beats. In some cases of heart failure, your heart muscle may become damaged and weakened, and the ventricles stretch (dilate) to the point that the heart can't pump blood efficiently throughout your body. Over time, the heart can no longer keep up with the normal demands placed on it to pump blood to the rest of your body.
An ejection fraction is an important measurement of how well your heart is pumping and is used to help classify heart failure and guide treatment. In a healthy heart, the ejection fraction is 50 percent or higher — meaning that more than half of the blood that fills the ventricle is pumped out with each beat. But heart failure can occur even with a normal ejection fraction. This happens if the heart muscle becomes stiff from conditions such as high blood pressure.
The term "congestive heart failure" comes from blood backing up into — or congesting — the liver, abdomen, lower extremities and lungs. However, not all heart failure is congestive. You might have shortness of breath or weakness due to heart failure and not have any fluid building up.
Heart failure can involve the left side (left ventricle), right side (right ventricle) or both sides of your heart. Generally, heart failure begins with the left side, specifically the left ventricle — your heart's main pumping chamber.
| Type of heart failure | Description |
|---|---|
| Left-sided heart failure | Fluid may back up in your lungs, causing shortness of breath. |
| Right-sided heart failure | Fluid may back up into your abdomen, legs and feet, causing swelling. |
| Systolic heart failure | The left ventricle can't contract vigorously, indicating a pumping problem. |
| Diastolic heart failure (also called heart failure with preserved ejection fraction) | The left ventricle can't relax or fill fully, indicating a filling problem. |
Any of the following conditions can damage or weaken your heart and can cause heart failure. Some of these can be present without your knowing it:
- Coronary artery disease and heart attack. Coronary artery disease is the most common form of heart disease and the most common cause of heart failure. Over time, arteries that supply blood to your heart muscle narrow from a buildup of fatty deposits — a process called atherosclerosis. The buildup of plaques can cause reduced blood flow to your heart.A heart attack occurs if plaques formed by the fatty deposits in your arteries rupture. This causes a blood clot to form, which may block blood flow to an area of the heart muscle, weakening the heart's pumping ability and often leaving permanent damage. If the damage is significant, it can lead to a weakened heart muscle.
- High blood pressure (hypertension). Blood pressure is the force of blood pumped by your heart through your arteries. If your blood pressure is high, your heart has to work harder than it should to circulate blood throughout your body.Over time, the heart muscle may become thicker to compensate for the extra work it must perform. Eventually, your heart muscle may become either too stiff or too weak to effectively pump blood.
- Faulty heart valves. The valves of your heart keep blood flowing in the proper direction through the heart. A damaged valve — due to a heart defect, coronary artery disease or heart infection — forces your heart to work harder to keep blood flowing as it should.Over time, this extra work can weaken your heart. Faulty heart valves, however, can be fixed or replaced if found in time.
- Damage to the heart muscle (cardiomyopathy). Heart muscle damage (cardiomyopathy) can have many causes, including several diseases, infections, alcohol abuse and the toxic effect of drugs, such as cocaine or some drugs used for chemotherapy.Genetic factors play an important role in several types of cardiomyopathy, such as dilated cardiomyopathy, hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy, left ventricular noncompaction and restrictive cardiomyopathy.
- Myocarditis. Myocarditis is an inflammation of the heart muscle. It's most commonly caused by a virus and can lead to left-sided heart failure.
- Heart defects you're born with (congenital heart defects).If your heart and its chambers or valves haven't formed correctly, the healthy parts of your heart have to work harder to pump blood through your heart, which, in turn, may lead to heart failure.
- Abnormal heart rhythms (heart arrhythmias). Abnormal heart rhythms may cause your heart to beat too fast, which creates extra work for your heart. Over time, your heart may weaken, leading to heart failure. A slow heartbeat may prevent your heart from getting enough blood out to the body and may also lead to heart failure.
- Other diseases. Chronic diseases — such as diabetes, HIV, hyperthyroidism, hypothyroidism, or a buildup of iron (hemochromatosis) or protein (amyloidosis) —also may contribute to heart failure.Causes of acute heart failure include viruses that attack the heart muscle, severe infections, allergic reactions, blood clots in the lungs, the use of certain medications or any illness that affects the whole body.
Risk factors
A single risk factor may be enough to cause heart failure, but a combination of factors also increases your risk.
Risk factors include:
- High blood pressure. Your heart works harder than it has to if your blood pressure is high.
- Coronary artery disease. Narrowed arteries may limit your heart's supply of oxygen-rich blood, resulting in weakened heart muscle.
- Heart attack. Damage to your heart muscle from a heart attack may mean your heart can no longer pump as well as it should.
- Diabetes. Having diabetes increases your risk of high blood pressure and coronary artery disease.
- Some diabetes medications. The diabetes drugs rosiglitazone (Avandia) and pioglitazone (Actos) have been found to increase the risk of heart failure in some people. Don't stop taking these medications on your own, though. If you're taking them, discuss with your doctor whether you need to make any changes.
- Certain medications. Some medications may lead to heart failure or heart problems. Medications that may increase the risk of heart problems include nonsteroidal anti-inflammatory drugs (NSAIDs); certain anesthesia medications; some antiarrhythmic medications; certain medications used to treat high blood pressure, cancer, blood conditions, neurological conditions, psychiatric conditions, lung conditions, urological conditions, inflammatory conditions and infections; and other prescription and over-the-counter medications.Don't stop taking any medications on your own. If you have questions about medications you're taking, discuss with your doctor whether he or she recommends any changes.
- Sleep apnea. The inability to breathe properly while you sleep at night results in low blood oxygen levels and increased risk of abnormal heart rhythms. Both of these problems can weaken the heart.
- Congenital heart defects. Some people who develop heart failure were born with structural heart defects.
- Valvular heart disease. People with valvular heart disease have a higher risk of heart failure.
- Viruses. A viral infection may have damaged your heart muscle.
- Alcohol use. Drinking too much alcohol can weaken heart muscle and lead to heart failure.
- Tobacco use. Using tobacco can increase your risk of heart failure.
- Obesity. People who are obese have a higher risk of developing heart failure.
- Irregular heartbeats. These abnormal rhythms, especially if they are very frequent and fast, can weaken the heart muscle and cause heart failure.
Complications
If you have heart failure, your outlook depends on the cause and the severity, your overall health, and other factors such as your age. Complications can include:
- Kidney damage or failure. Heart failure can reduce the blood flow to your kidneys, which can eventually cause kidney failure if left untreated. Kidney damage from heart failure can require dialysis for treatment.
- Heart valve problems. The valves of your heart, which keep blood flowing in the proper direction through your heart, may not function properly if your heart is enlarged or if the pressure in your heart is very high due to heart failure.
- Heart rhythm problems. Heart rhythm problems (arrhythmias) can be a potential complication of heart failure.
- Liver damage. Heart failure can lead to a buildup of fluid that puts too much pressure on the liver. This fluid backup can lead to scarring, which makes it more difficult for your liver to function properly.
Some people's symptoms and heart function will improve with proper treatment. However, heart failure can be life-threatening. People with heart failure may have severe symptoms, and some may require heart transplantation or support with a ventricular assist device.
Treatments and drugs
Heart failure is a chronic disease needing lifelong management. However, with treatment, signs and symptoms of heart failure can improve, and the heart sometimes becomes stronger. Treatment may help you live longer and reduce your chance of dying suddenly.
Doctors sometimes can correct heart failure by treating the underlying cause. For example, repairing a heart valve or controlling a fast heart rhythm may reverse heart failure. But for most people, the treatment of heart failure involves a balance of the right medications and, in some cases, use of devices that help the heart beat and contract properly.
Medications
Doctors usually treat heart failure with a combination of medications. Depending on your symptoms, you might take one or more medications, including:
- Angiotensin-converting enzyme (ACE) inhibitors. These drugs help people with systolic heart failure live longer and feel better. ACE inhibitors are a type of vasodilator, a drug that widens blood vessels to lower blood pressure, improve blood flow and decrease the workload on the heart. Examples include enalapril (Vasotec), lisinopril (Zestril) and captopril (Capoten).
- Angiotensin II receptor blockers. These drugs, which include losartan (Cozaar) and valsartan (Diovan), have many of the same benefits as ACE inhibitors. They may be an alternative for people who can't tolerate ACE inhibitors.
- Beta blockers. This class of drugs not only slows your heart rate and reduces blood pressure but also limits or reverses some of the damage to your heart if you have systolic heart failure. Examples include carvedilol (Coreg), metoprolol (Lopressor) and bisoprolol (Zebeta).These medicines reduce the risk of some abnormal heart rhythms and lessen your chance of dying unexpectedly. Beta blockers may reduce signs and symptoms of heart failure, improve heart function, and help you live longer.
- Diuretics. Often called water pills, diuretics make you urinate more frequently and keep fluid from collecting in your body. Diuretics, such as furosemide (Lasix), also decrease fluid in your lungs so you can breathe more easily.Because diuretics make your body lose potassium and magnesium, your doctor also may prescribe supplements of these minerals. If you're taking a diuretic, your doctor will likely monitor levels of potassium and magnesium in your blood through regular blood tests.
- Aldosterone antagonists. These drugs include spironolactone (Aldactone) and eplerenone (Inspra). These are potassium-sparing diuretics, which also have additional properties that may help people with severe systolic heart failure live longer.Unlike some other diuretics, spironolactone and eplerenone can raise the level of potassium in your blood to dangerous levels, so talk to your doctor if increased potassium is a concern, and learn if you need to modify your intake of food that's high in potassium.
- Inotropes. These are intravenous medications used in people with severe heart failure in the hospital to improve heart pumping function and maintain blood pressure.
- Digoxin (Lanoxin). This drug, also referred to as digitalis, increases the strength of your heart muscle contractions. It also tends to slow the heartbeat. Digoxin reduces heart failure symptoms in systolic heart failure. It may be more likely to be given to someone with a heart rhythm problem, such as atrial fibrillation.
You may need to take two or more medications to treat heart failure. Your doctor may prescribe other heart medications as well — such as nitrates for chest pain, a statin to lower cholesterol or blood-thinning medications to help prevent blood clots — along with heart failure medications.
You may be hospitalized if you have a flare-up of heart failure symptoms. While in the hospital, you may receive additional medications to help your heart pump better and relieve your symptoms. You may also receive supplemental oxygen through a mask or small tubes placed in your nose. If you have severe heart failure, you may need to use supplemental oxygen long term.
Surgery and medical devices
In some cases, doctors recommend surgery to treat the underlying problem that led to heart failure. Some treatments being studied and used in certain people include:
- Coronary bypass surgery. If severely blocked arteries are contributing to your heart failure, your doctor may recommend coronary artery bypass surgery. In this procedure, blood vessels from your leg, arm or chest bypass a blocked artery in your heart to allow blood to flow through your heart more freely.
- Heart valve repair or replacement. If a faulty heart valve causes your heart failure, your doctor may recommend repairing or replacing the valve. The surgeon can modify the original valve (valvuloplasty) to eliminate backward blood flow. Surgeons can also repair the valve by reconnecting valve leaflets or by removing excess valve tissue so that the leaflets can close tightly. Sometimes repairing the valve includes tightening or replacing the ring around the valve (annuloplasty).Valve replacement is done when valve repair isn't possible. In valve replacement surgery, the damaged valve is replaced by an artificial (prosthetic) valve.Certain types of heart valve repair or replacement can now be done without open heart surgery, using either minimally invasive surgery or cardiac catheterization techniques.
- Implantable cardioverter-defibrillators (ICDs). An ICD is a device similar to a pacemaker. It's implanted under the skin in your chest with wires leading through your veins and into your heart.The ICD monitors the heart rhythm. If the heart starts beating at a dangerous rhythm, or if your heart stops, the ICD tries to pace your heart or shock it back into normal rhythm. An ICD can also function as a pacemaker and speed your heart up if it is going too slow.
- Cardiac resynchronization therapy (CRT), or biventricular pacing. A biventricular pacemaker sends timed electrical impulses to both of the heart's lower chambers (the left and right ventricles) so that they pump in a more efficient, coordinated manner.Many people with heart failure have problems with their heart's electrical system that cause their already-weak heart muscle to beat in an uncoordinated fashion. This inefficient muscle contraction may cause heart failure to worsen. Often a biventricular pacemaker is combined with an ICD for people with heart failure.
- Heart pumps. These mechanical devices, such as ventricular assist devices (VADs), are implanted into the abdomen or chest and attached to a weakened heart to help it pump blood to the rest of your body. VADs are most often used in the heart's left ventricle, but they can also be used in the right ventricle or in both ventricles.Doctors first used heart pumps to help keep heart transplant candidates alive while they waited for a donor heart. VADs are now sometimes used as an alternative to transplantation. Implanted heart pumps can significantly extend and improve the lives of some people with severe heart failure who aren't eligible for or able to undergo heart transplantation or are waiting for a new heart.
- Heart transplant. Some people have such severe heart failure that surgery or medications don't help. They may need to have their diseased heart replaced with a healthy donor heart.Heart transplants can dramatically improve the survival and quality of life of some people with severe heart failure. However, candidates for transplantation often have to wait a long time before a suitable donor heart is found. Some transplant candidates improve during this waiting period through drug treatment or device therapy and can be removed from the transplant waiting list.
End-of-life care and heart failure
Even with the number of treatments available for heart failure, it's possible that your heart failure may worsen to the point where medications are no longer working and a heart transplant or device isn't an option. If this occurs, you may need to enter hospice care. Hospice care provides a special course of treatment to terminally ill people.
沒有留言:
張貼留言